It is now just over a week since I marched at my Commencement ceremony and received my diploma. Yes, the actual diploma was inside the folder — which is very exciting since all my previous diplomas (college and high school) had to be mailed to me once the financial office had decided that I no longer owed the school any money.
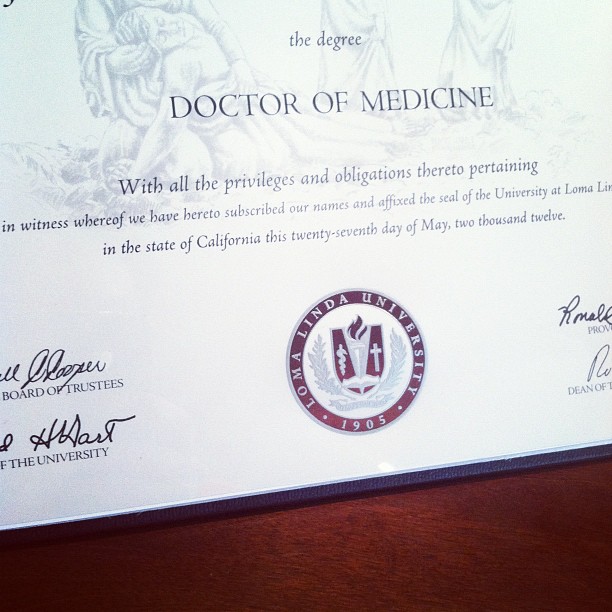
I suppose that this is officially my first post as an MD. I am now a graduate. I now can tack on the suffix M.D. to my name. I remember just one day after graduation I sat staring at my diploma. As I stared at it, I almost could not believe it was in front of me. I looked at the piece of paper — a sheet of paper that has been the most expensive (physically, mentally, spiritually, and emotionally) paper I have ever earned.
During the days prior to graduation, I remember feeling excited. At the same time, I also felt nervous. Nervous about being done. Nervous about new responsibilities. Nervous about wearing the long white coat I have wanted ever since I looked into the mirror and saw how ridiculous my short white coat looked. I am now waiting for my long coat. Literally. I sent an email to the Graduate Medical Education (GME) office a few weeks ago with my size. I hope I sent in the right size. Again, I am excited. But again, I am nervous about the long white coat and all the responsibility it represents.
I have a few more weeks before residency starts and I step onto the wards as a new intern. During this time I will have to complete some online modules and get certified for Advanced Cardiac Life Support (ACLS). I will also complete my move into a new place. It is a few weeks that I know will go by very quickly. Actually, I feel like the next few years will go quickly, but I don’t really want to think about that at this point.
And so, my medical school career is over. One chapter is completed. But I know that I am far from the end. Medical training continues at the next stage — residency. I know, too, that it will continue long after I leave residency. Medicine, as they have taught me throughout medical school, is about lifelong learning. In the grand scheme of things, I am still at the beginning. I have “leveled up,” but I’m still at a very low level.
I have a long way to go. I know the road ahead will be hard. But it’ll be full of adventure, I’m sure.
I will continue to blog here. For those of you who have been following my journey thus far, I hope you stick around.




